




Support groups aren’t just helpful—they’re clinically proven. With rising mental health demands and limited health care resources, professionals are turning to support groups as a powerful, scalable solution. Backed by the latest outcomes research, these groups do more than offer emotional relief—they improve psychological and functional health care outcomes, build resilience, and create a lasting sense of community.
In this blog, we’ll break down key findings from recent peer-reviewed journals and show you how to apply them in practice. From designing effective group structures to sustaining engagement, you’ll gain practical, research-backed strategies to enhance patient care and expand your impact, especially in areas like substance abuse, bipolar disorder, or body dysmorphic disorder, where healthcare providers seek comprehensive, community-based solutions.
Support groups are more than just a space for conversation—they offer measurable benefits that contribute to improved mental health outcomes. Recent research highlights how both peer-led and professionally facilitated support groups positively impact psychological well-being, stress management, and overall quality of life.
A recent evaluation of PeerTalk, a peer-led mental health support service, found that participants experienced significant improvements in mental well-being. The study highlighted several key factors contributing to these positive outcomes:
The study reinforced a key insight: peer support groups complement formal mental health treatment but do not replace it. While they provide emotional safety and ease of access, they are most effective when integrated alongside professional care.
A systematic review of professionally led cancer support groups further supports the effectiveness of structured group interventions. Across multiple studies, these groups were linked to reductions in:
Beyond symptom reduction, participants reported additional benefits:
The review also identified critical factors for successful implementation:
The connection between social support and stress reduction is well-documented. Acoba’s 2024 study, based on Lazarus and Folkman’s Stress and Coping Theory, examined how different types of social support influence mental health outcomes.
Findings showed that perceived stress mediated the effect of social support on:
One key discovery was that family and significant other support had the strongest impact on reducing perceived stress, leading to better mental health outcomes. Interestingly, the study found that friend support alone was not a significant stress buffer, suggesting that deeper, more stable social connections may play a greater role in stress reduction.
By understanding these findings, mental health professionals can better integrate support groups into their practice, ensuring that clients receive the right type of group intervention to meet their needs.
Support groups are effective because they tap into core psychological and behavioral mechanisms that drive positive change. Research highlights four key ways in which these groups improve mental health outcomes.
How individuals interpret and respond to stress significantly impacts their mental health. Acoba (2024) found that peer support alters stress appraisal, helping individuals reframe challenges and perceive them as more manageable. When people share their experiences and receive validation, they often feel less overwhelmed by their problems. This shift in perception can reduce anxiety and improve coping abilities, an effect aligned with stress management.
A common challenge for individuals facing mental health conditions is social isolation. The PeerTalk evaluation (Beard et al., 2024) emphasized how group participation fosters a sense of connection. Talking with others who have similar experiences reduces loneliness and enhances emotional insight, allowing individuals to better understand their own emotions through shared narratives. This sense of belonging is especially important for patients navigating grief, substance abuse, or bipolar disorder.
Support groups encourage active engagement and accountability. Group members often model positive coping behaviors, motivating others to take action. Whether it is attending therapy sessions, practicing self-care, or engaging in stress-reducing activities, seeing others succeed increases the likelihood of participants adopting similar behaviors. Regular meetings reinforce consistency, which is crucial for long-term mental health improvement.
A key outcome of structured support groups, particularly professionally facilitated ones (Li et al., 2024), is increased self-efficacy—the belief in one's ability to manage their own condition. By providing education, strategies, and encouragement, support groups help participants feel more in control of their treatment journey, strengthening their ability to make informed health decisions.
For mental health professionals looking to integrate support groups into their practice, designing an effective program requires careful planning. The following best practices ensure that groups are structured, impactful, and sustainable.
A well-structured support group begins with a clear purpose and format. Consider:
The effectiveness of a support group often depends on skilled facilitation. Facilitators, whether peers or professionals, should have:
Not every individual is suited for a support group setting. A screening process helps align participant needs with group objectives. Key considerations include:
Continuous assessment ensures the group remains effective. Professionals can use validated tools to measure:
By understanding the mechanisms behind why support groups work and implementing best practices, mental health professionals can create programs that are structured, effective, and research-backed. Well-designed support groups not only provide emotional relief but also empower individuals to take control of their mental health while complementing formal treatment approaches.

While support groups offer significant benefits, their success depends on proper structure and management. Without clear guidelines, groups can face challenges that undermine their effectiveness. Mental health professionals should be aware of these common pitfalls to ensure support groups remain safe, supportive, and impactful.
A well-functioning online support group requires clear goals, rules, and expectations for both participants and facilitators. Without structure, discussions may become unfocused, leading to frustration or disengagement. Groups should have:
Trust is the foundation of any peer support group. If participants feel their privacy is at risk, they may hesitate to share openly. Facilitators should:
Peer-led groups provide valuable shared experiences, but they also risk spreading inaccurate health information. Without professional oversight, participants may unintentionally share misleading advice. To mitigate this:
Facilitators—whether peer or professional—play a crucial role in maintaining group effectiveness. However, without proper support, they may experience burnout, leading to reduced effectiveness or even group dissolution. To prevent this:
Support groups are most effective when they complement formal treatment. However, if they operate in isolation, participants may miss out on more comprehensive care. Mental health professionals should:
For mental health professionals looking to expand the impact of support groups, integration into clinical and community settings is key. By leveraging research-backed strategies, clinicians can enhance accessibility, secure funding, and increase engagement while maintaining quality care.
Clinicians should share evidence-based insights with healthcare professionals, social workers, and potential participants. Research-backed statistics—such as reductions in stress, improved mood, or increased empowerment—help establish credibility and encourage referrals. This can be done through:
Support groups often require financial resources for facilitators, training, and operational costs. Many healthcare grants fund community-based mental health programs, especially those with proven outcomes. To increase funding opportunities:
Support groups can become an essential part of hospital programs, outpatient clinics, and mental health organizations. To integrate them effectively:
Many organizations already run successful peer support group models. Mental health professionals can partner with existing networks rather than starting from scratch. Examples include:
While marketing is important for participant engagement, ethical considerations must come first. Support groups should be promoted transparently, without overpromising results. Effective outreach strategies include:
Scaling and integrating support groups requires a strategic approach that balances accessibility, funding, and professional oversight. By leveraging research findings, advocating for inclusion within healthcare systems, and maintaining ethical promotion, mental health professionals can expand the reach and effectiveness of these valuable community-based interventions.
The research is clear—peer support groups work. From reducing anxiety and stress to boosting confidence and connection, well-run support groups are a proven way to strengthen mental health outcomes. They don’t replace therapy—they enhance it.
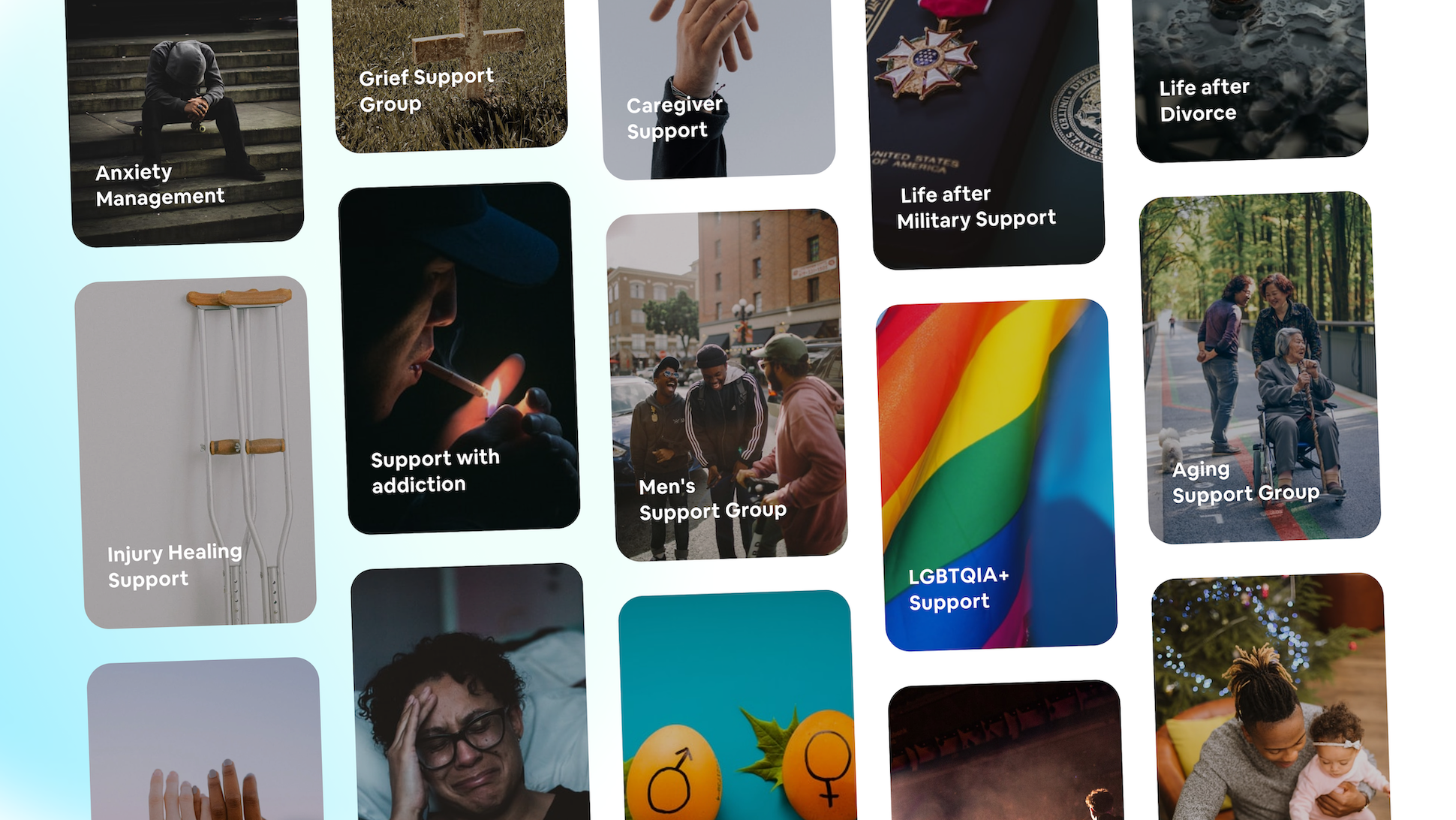
As a health care provider or mental health professional, you have the chance to create safe spaces where healing happens together. Whether you're supporting individuals with substance abuse, bipolar disorder, or addiction, or helping caregivers and parents, these groups can complement formal care and reinforce outcomes research.
Whether you're just getting started or looking to level up an existing group, MentalHappy.com has the tools and support to help you succeed. With resources backed by insights from organizations like the Anxiety and Depression Association of America, Mayo Clinic, and the American Psychological Association, your impact can reach further than ever.
Ready to turn shared struggles into shared strength?

If you are in a life-threatening situation - DO NOT use this platform.
Use these resources to get immediate help.


